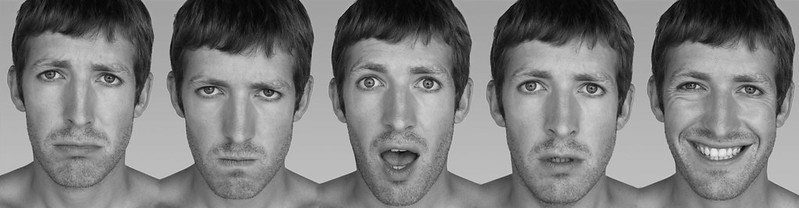
What are psychosomatic mechanisms? How can emotions lead to physical changes in the body? Body function changes when we experience strong emotions, as we are all aware. These changes include rapid heartbeat, perspiration, breathlessness, and trembling in association with fright. Symptoms of sustained nervous tension, e.g., diarrhea, frequency of urination, headache, nausea, indigestion, etc., experienced before significant examinations, interviews, etc., are part of everyone’s experience.
Extensive and meticulous studies have been carried out both in animals and in humans, and it has been possible to measure and describe functional changes in most major systems of the body under acute and chronic stress. These changes constitute normal physiological adaptation to stress and can be regarded as mechanisms that prepare the organism to cope with danger. For example, Walter B. Cannon regarded the immediate physiologic alterations occurring in frightened animals as preparation for the muscular exertion of “fight or flight.”
Alterations in function accelerate and redistribute circulating blood, ensuring that more of it gets to where it is needed. The skeletal muscles and vital organs (heart, lungs, and brain) receive most of the oxygen under these conditions, while the skin and digestive system are less strained.
Franz Alexander, a leading clinical theorist, has suggested that chronically sustained emotions may accompany chronically sustained physiological changes. This means that a continuing state of anger may be accompanied by a continuing elevation of blood pressure. Thousands of tiny arterial vessels (arterioles) throughout the body can narrow and cause spasms, causing an acute rise in blood pressure.

In most cases, these vessels relax and the blood pressure returns to normal when the acute emotional state has passed. If for psychological reasons the emotion cannot be adequately expressed in speech or action, Alexander theorizes that the physiologic constriction of the arterioles will persist and that the sustained contraction (and elevated pressure) may then lead to permanent changes (narrowing and stiffening of these vessels), which from then on would provide a structural basis for hypertension.
Similarly, he feels that chronically maintained excessive acid production by the stomach in association with unresolved emotions may contribute to the formation of an ulcer in the lining of the stomach (peptic ulcer). These statements represent only a part of Alexander’s theories which, in their entirety, encompass a lot more. They are mentioned here as representative of the concept (shared by many investigators) that changes in body function, ordinarily normal adaptive accompaniments to emotion, may, if exaggerated and sustained, become maladaptive.
If exaggerated for too long, they might contribute to irreversible structural changes in body tissue. Based on what we know, this is how it could happen. The exact way it happens is still unknown. WHM determines which disease a person will get. Do certain specific emotional problems lead to specific diseases or can strong unresolved psychological conflict lead to any one of these diseases There has been and continues to be a lot of controversy about this issue. Eminent authorities take opposite positions about this question. (When this is the case, it usually means the answer is not yet known.)
On the one hand, there are some who consider that body function changes that accompany emotional arousal, such as those described above, are nonspecific. They also believe that physical disease developing under sustained emotional tension will occur in whatever organs are most vulnerable because of hereditary or constitutional factors. In other words, when the organism is put under stress, trouble will develop at the “weakest link in the chain.”
On the other hand, many clinicians and investigators feel that there are important differences in the psychological sphere between patients with different “psychosomatic diseases” and postulate that each different emotion is accompanied by its own specific pattern of physiologic arousal and so consider that the type of emotional conflict plays a role in determining which tissues will be damaged and hence which disease will develop.
In the examples cited above, it is implied that conflicts having to do with the expression and discharge of anger would be more likely to activate a disease of the cardiovascular system such as hypertension, whereas conflicts around receiving love and being cared for, would be more likely to interfere with stomach function and lead to a disease such as a peptic ulcer.
Although a lot of research has been directed at this issue, the findings are not clear-cut and advocates of each point of view can find partial support in the results. Most physicians interested in this field, but not actively partisan in the controversy, consider the question is still open. They tend to feel that the truth lies somewhere in between. Compromise theories that consider both constitutional-genetic and psychological factors as determinants of the choice of disease have been advanced by many investigators, including Franz Alexander, I. Arthur Mirsky, Roy R. Grinker, Felix Deutsch, and others.
The critical point to emphasize here is that emotional factors may contribute to the development of certain diseases and influence their course. However, a full explanation of the mechanisms involved has not yet been achieved. Some people have persistent and recurrent physical symptoms such as headaches for which the doctor can find no physical basis. Are such symptoms “imaginary” because they are “all in the mind?” No pain or bodily discomfort is ever “imaginary.”
Many such symptoms actually originate from functional rather than structural bodily changes. For example, a large proportion of headaches arise as the result of tension (mild sustained contraction) of the muscles of the neck and scalp that leads to soreness and pain originating in these muscles.
This pain is just as real as that arising from a tumor that can be seen or palpated (examined by the hand), or otherwise detected by special laboratory examination such as an X-ray. Similarly, diarrhea and abdominal cramps that result from disturbed circulation and muscle tone in the intestines do not feel different from diarrhea resulting from bowel infection. In some cases, there is no demonstrable functional disturbance in the body tissues.
In these instances, pain and discomfort arise from purely psychological mechanisms such as conversion hysteria. The symptoms and discomfort remain real to the patient. It should be remembered that the psychological processes underlying such symptoms are outside the patient’s conscious purview and voluntary control. In other words, the symptom is imposed upon the patient by forces beyond his control. It is experienced when a part of the body is injured, diseased, or functioning improperly.
Read More: What is Anger – The Unrecognized Emotion