What is Malignant Pleural Mesothelioma
It is a rare but fatal tumor caused mainly by asbestos exposure. There is no standard treatment as mesothelioma is primarily resistant to all treatments including chemotherapy. Asbestos-induced oxidative stress is thought to play an essential role in the pathogenesis of mesothelioma in the process possibly increasing the expression of the major antioxidant defense mechanisms of the cells.
Both chemo and radiotherapy act at least partly by provoking reactive oxygen species (ROS) generation suggesting a role for the intracellular antioxidants in drug resistance. Other mechanisms associated with drug resistance include the plasma membrane drug transporters, of which several are also redox-regulated.
In the expression and possible role of the major antioxidant enzymes (AOEs), the manganese superoxide dismutase (MnSOD), catalase, and mechanisms closely related to glutathione (GSH) metabolism were investigated in the biopsies of Malignant Pleural Mesothelioma and/or cell lines in culture.
The methods included Northern Blotting, Western Blotting analysis, immunohistochemistry, and measurement of specific enzyme activities. Cell damage after oxidant or cytotoxic drug exposures was analyzed by lactate dehydrogenase release, depletion of high-energy nucleotides, and microculture tetrazolium dye assay. MnSOD was highly expressed in mesothelioma tumor biopsies in vivo and cell lines in vitro-compared to non-malignant mesothelial cells.
Mesothelioma cell line expressing the highest MnSOD (10 fold compared to non-malignant mesothelial cells) levels also had the highest levels of GSH, glutathione S-transferase (GST), and catalase, and was the most resistant cell line to oxidants and cytotoxic drugs.
In contrast to mesothelioma cells, lung A549 adenocarcinoma cells, which represent an oxidant and drug-resistant cell line, contained similar levels of MnSOD as non-malignant mesothelial cells. They, however, also contained higher intracellular GSH levels and catalase than mesothelioma cells and had elevated levels of γ-glutamylcysteine synthetase (γGCS). The rate-limiting enzyme in GSH biosynthesis. in contrast to tumor necrosis factor-α (TNFα), cytotoxic drugs failed to induce MnSOD mRNA, protein, or activity in A549 cells.
The endogenous level of MnSOD or its induction by TNFα did not explain the oxidant resistance of these cells. GST could not explain the resistance of adenocarcinoma cells. Is the activity of total GST lower in adenocarcinoma cells than in more sensitive mesothelioma cells?
The role of GSH and catalase were also investigated by treating the Malignant Pleural Mesothelioma cells and A549 adenocarcinoma cells with buthionine sulfoximine (BSO), to block glutathione synthesis, and aminotriazole (ATZ) to inhibit catalase. Both BSO – and ATZ – treatment enhanced H2O2 toxicity in three mesothelioma cell lines. While only the depletion of glutathione increased epirubicin toxicity.
BSO treatment also significantly potentiated cisplatin-induced cytotoxicity in mesothelioma and adenocarcinoma cells. Given the obvious importance of GSH in the oxidant and drug resistance of these tumors, altogether 34 mesothelioma tumor biopsies were investigated for both subunits of γGCS.
The catalytic, heavy subunit of γGCS was highly expressed in most of the cases, whereas the regulatory, light subunit (γGCSl) expression was weaker. No expression of these proteins could be detected from the non-malignant mesothelium. The integral membrane drug transporter, P-glycoprotein (P-gp), immunopositivity was found in 61 %, and multidrug resistance proteins 1 and 2 (MRP1 and MRP2) immune positivity in 58 % and 33 % of 36 mesothelioma biopsies.
Normal mesothelium did not express these multidrug-resistant proteins. There was no significant association between tumor proliferation, apoptosis or patient survival and expression of the multidrug-resistant proteins. In conclusion, the simultaneous induction of multiple antioxidant enzymes can occur in human mesothelioma cells.
In addition to the high MnSOD activity, H2O2-scavenging antioxidant mechanisms, γGCS, GST and GSH can partly explain the high oxidant and drug resistance of these cells in vitro; the role of catalase during heavy oxidant exposure is possible. MnSOD can be induced by TNFα, but the induction, however, does not provide any protection against repeated oxidant exposures.
Many mechanisms contributing to the resistance of mesothelioma remain to be investigated, but γGCS may play an important role in the primary drug resistance of this tumor in vivoin maintaining the intracellular glutathione level. The multidrug resistance proteins P-gp, MRP1, and MRP2 are expressed in Malignant Pleural Mesothelioma cells but are not likely to be responsible for the primary drug resistance of this malignancy.
Mesothelioma is a tumor derived from the serosal lining of the pleural, peritoneal, or pericardial cavities and is most commonly situated in the pleura. Malignant Pleural Mesothelioma are rare tumor, accounting for only about 1% of all cancer deaths in the world. Pleural mesothelioma is in approximately 85-90% of cases an asbestos-initiated lethal malignancy. The latency period is about 20 to 40 years.
Accordingly, the peak in mesothelioma cases is expected in 2010, although the asbestos usage in most industrialized countries has been abolished since the 1980s. The prognosis of mesothelioma is poor, as it is highly invasive and primarily resistant to all treatments. Which is including radiotherapy and cytotoxic drugs. A major factor in the pathogenesis has been considered asbestos-induced oxidative stress, which in turn is known to induce several antioxidant mechanisms in the cells.
Mesothelioma provides a vital model for cancer research of a therapy-resistant malignancy in which antioxidant mechanisms may at least partly explain the resistance. Intracellular antioxidants offer protection not only against reactive oxygen species (ROS) but may also modulate the response to different chemotherapeutic drugs that are used in cancer treatment.
Manganese superoxide dismutase (MnSOD) scavenges superoxide radicals and has a controversial role in cancer biology. It has been suggested to be a cancer suppressor. But on the other hand, it offers protection against oxidative stress and thereby may confer resistance against oxidant-producing drugs. MnSOD is overexpressed in only some malignant tumors, but its importance in drug resistance is unsolved.
Glutathione has in many studies been linked with drug resistance both for its role as an antioxidant and also for its function in detoxification reactions. Attention has been drawn to the enzymes in glutathione biosynthesis and how the cell maintains its glutathione level.
Several studies have also been done with other mechanisms that utilize intracellular glutathione and transport it extracellularly. Glutathione S-transferases are a family of detoxification enzymes that are often associated with chemoresistance.
However, the activity of these enzymes is unidentified in Malignant Pleural Mesothelioma. Even though polymorphism of GSTM1 has been linked to the development of this disease. Catalase in addition to glutathione takes part in scavenging excess hydrogen peroxide in the cells. Not many studies link it to drug resistance of malignant cells, but its role should be clarified in oxidant and drug resistance of mesothelioma.
The classical inducers of multidrug resistance are the drug export pumps in the plasma membrane that have different substrate specificities. P-glycoprotein has been studied most, but the recently discovered MRP family offers new avenues for investigators in cancer biology. The first members in the MRP family, MRP1 and MRP2, are dependent on intracellular glutathione and they transport glutathione-conjugated substrates.
In Malignant Pleural Mesothelioma, these mechanisms have not been thoroughly studied before. This series of studies was designed to systematically investigate the expression of the most important antioxidant pathways and drug transporters in mesothelioma cells in vitro and tumor biopsies in vivo.
Besides investigating the expression of these mechanisms, their role in oxidant and chemotherapeutic drug resistance was assessed in vitro. The expression of the AOEs and related proteins was also correlated with tumor growth and patient survival.
History
In 1767 J. Lieutaud recognized two pleural tumors in a series of autopsies, but Wagner was the first to describe the pathology of a primary malignant pleural tumor in 1870. The term mesothelioma was first used by Eastwood and Martin in 1921.
In 1960 Wagner reported 33 cases of diffuse pleural mesothelioma in South Africa, in an area of crocidolite mining. Of these 33 patients, 32 had a history of asbestos exposure and this connected mesothelioma with asbestos. The first reports of mesothelioma in Finland are from the 1960s.
Epidemiology
Mesothelioma is a rare disease, but its incidence keeps increasing despite the industrial restriction of asbestos usage from the 1980s, as the latency period is approximately 20 -40 years. About 70 cases of mesothelioma are diagnosed in Finland every year.
It has been estimated that the peak of mesothelioma incidence in Finland will be around 2010, with approximately 100 cases per year. The peak incidence has been already achieved in the U.S, but e.g. in Britain, the number of cases per year is climbing and is expected to increase to more than 3000 cases per year.
Malignant Pleural Mesothelioma is more common among men, only about 10% occur in women. In about 80-90% of the male cases, obvious asbestos exposure is known. In females, it has been suggested that only 23% of mesothelioma cases are asbestos-related. Sporadic cases among children and infants occur.
Etiology
Asbestos is the single most important causative agent of mesothelioma, and exposure to asbestos fibers is usually occupational. Other lung diseases are caused by asbestos as well, including asbestosis, lung cancer, pleural plaques, pleural fibrosis, pleural effusions, and pseudotumors. Factors determining the risk of mesothelioma include the fiber type, time from exposure, fiber dimensions, and fiber surface properties.
There is evidence that persons with greater intensity and duration of asbestos exposure have a higher risk for mesothelioma which, however, can develop with minimal exposure. Therefore, the causative role of asbestos is difficult to rule out as most adults in the industrialized world have asbestos in their lungs. Fibers greater than 8 μm in diameter are most commonly associated with mesothelioma.
Asbestos is a commercial term for a variety of naturally occurring hydrated fibrous silicates. The material is subdivided into two groups, serpentine fibers, and amphiboles. The capacity of different types of asbestos fibers to induce mesothelioma seems to be greatest with amphiboles like amosite (“brown asbestos”) and crocidolite (“blue asbestos”), whereas the serpentine fiber chrysotile (“white asbestos”) is not as tumorigenic.
Chrysotile comprises 90% of the asbestos used worldwide. In Finland, however, the main asbestos used has been anthophyllite, which is one of the amphiboles. It is associated with asbestos-induced diseases such as asbestosis and pleural plaques. Mesothelioma cases are rare, but some have been reported.
Non-asbestos causes of mesothelioma have not been revealed in epidemiological studies, but theoretically, any agent injuring pleura may cause mesothelioma. These include chemical agents, chronic inflammation, viruses, and radiation. Smoking does not increase the risk of mesothelioma. A possible connection to Simian Virus 40 (SV40) was suggested.
In the late 1950s and the early 1960s polio vaccines were contaminated with SV40 and millions of people were exposed. In Finland, vaccines were not contaminated and none of the mesothelioma patients in Finland had received a contaminated vaccine. SV40 large T-antigen has been detected in a high proportion of mesothelioma tissue specimens. However, other SV40-like DNA sequences were also found in non-malignant pleural diseases.
The role of SV40 is unclear, even though in the United States and many other parts of Europe the consensus seems to link it to Malignant Pleural Mesothelioma. Genetic susceptibility is associated at least with some detoxification enzyme polymorphisms. That is including the homozygous deletion of the GSTM1 gene or slow acetylation-associated N-acetyl transferase-2 (NAT2) genotype.
Pathogenesis and pathology
The inhaled asbestos fibers must be transported to the pleural cavity to reach the target cells. Parietal pleura are often more extensively involved, but usually, it is difficult to determine if mesotheliomas begin in the visceral or parietal pleura. When inhaled into the respiratory bronchioles and alveoli, chrysotile fibers are usually fragmented by organic acids and cleared by macrophages.
Amphiboles are not as easily decomposed and may remain unchanged for years/decades. The asbestos fibers are transported to the pleural cavity via the lymphatic pathway or by penetrating the visceral pleura. Amphibole fibers concentrate on certain areas of the parietal pleura, called black spots, that are openings of lymph vessels, and at these spots, the pleura is exposed for years to the effects of asbestos fibers and toxic reactive oxygen species (ROS).
Free radicals and other toxic oxygen metabolites are considered important in the pathogenesis of mesothelioma. Fibers themselves have redox properties as they contain ferrous iron which catalyzes the reaction forming ROS.
ROS are also formed indirectly when phagocytic cells meet the fibers; macrophages and neutrophils are known to liberate ROS after asbestos exposure. These active oxygen intermediates can participate in the oncogenic process by many different mechanisms. Genotoxicity, lipid peroxidation, and oncogene modulation are all possible effects of ROS. The long latency period suggests cumulative genetic, cytotoxic, and proliferative events.
Malignant Pleural Mesothelioma is divided histologically into three classes (Travis et al., 1999). The epithelial subtype comprises about 54% of all mesothelioma cases. Epithelial mesotheliomas may be predominantly composed of acinar structures, and differential diagnosis from adenocarcinoma is often demanding.
Other variants of epithelial mesothelioma also exist. Sarcomatoid mesotheliomas, which histologically resemble fibrosarcomas, represent approximately 20% of the cases, and the rest of the cases fall into biphasic mesotheliomas, representing about 25% of the cases.
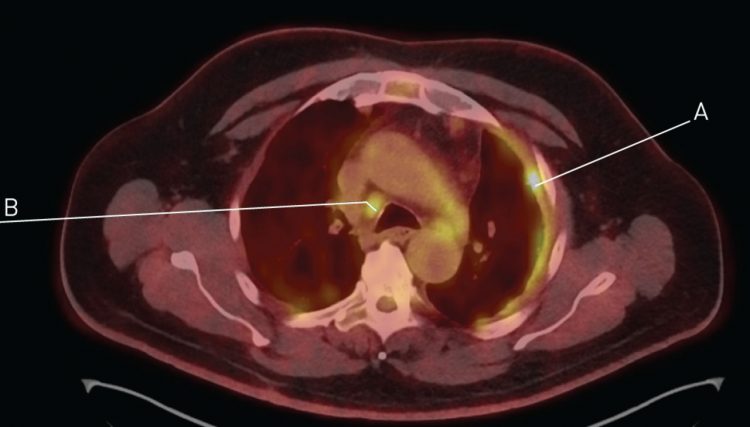
Clinical features and diagnosis the average age of a patient at the time of diagnosis are approximately 60 years, and there is a strong male predominance. The first symptoms include chest pain, dyspnea, weakness, and cough. Usually, the diagnosis is delayed due to the non-specificity of the symptoms. Thoracic radiograph initially shows pleural effusion in 92% of cases, usually on one side. Only 7 % of a multinodular pleural tumor without fluid is seen.
In early cases of Malignant Pleural Mesothelioma, nodules or plaques of varying sizes can be detected in the parietal pleura. Serosal thickening and consequent effusion are often marked. Most cases are unicavitary. Mesothelioma seldom sends metastasis, but it is highly invasive, e.g. to the pericardium.
One of the first diagnostic procedures is cytology of pleural fluid which gives positive results in approximately 30% of cases. Another method used for a diagnostic workup is the computed tomography (CT) scan. The diagnosis is established by biopsy via thoracoscopy in most of cases. Examination of biopsy of parietal and visceral pleura is the most reliable method for diagnosis.
Histological diagnosis is, however, difficult because of structural variability between different tumors and even within the same tumor, the main problem being differential diagnosis from metastatic adenocarcinoma of the lung. Other differential diagnostic difficulties arise from benign mesothelial hyperplasia and sarcomas in cases of sarcomatoid mesothelioma. In addition to the typical histopathology, a panel of immunohistochemical stains will often suggest the right diagnosis.
Many antigens stain positively in adenocarcinoma but remain negative in mesothelioma. The markers used in the diagnostic procedure include the carcinoembryonic antigen (CEA), glycoprotein markers Leu-M1, Ber-EP4, and B72.3, and others like epithelial marker antigen (EMA) and human milk fat globulin-2 (HMFG-2).
In epithelioid tumors, diastase-resistant neutral mucin is positive in approximately 70% of adenocarcinomas, but usually negative in epithelial mesothelioma. In the case of sarcomatoid mesothelioma cytokeratins like CK 5/6 and AE1/AE3 are used, as they are generally positive in sarcomas and negative in sarcomatoid mesothelioma.
Calretinin, which reveals the mesothelial origin, is usually positive in mesothelioma and negative in sarcoma and its specificity is over 90%. In differentiating between reactive and neoplastic mesothelium attention should be focused on the degree of cellular atypia and the presence of collagen necrosis that are highly suggestive of malignancy.
Treatment and Prognosis
Treatment of malignant mesothelioma remains disappointing, and there is no standard treatment. As in other malignant tumors, surgery, radiation therapy, chemotherapy, supportive therapy, or a combination of different modalities are used.
No treatment has so far been shown to offer better survival than supportive therapy alone. The median survival time from diagnosis is less than one year, and 5-year survival is less than 5 %. Some factors, however, indicate a more favorable prognosis, including epithelial subtype, age < 65 years, good clinical condition with no weight loss, and absence of visceral pleura involvement.
Surgery alone does not improve survival but may be beneficial for palliation. Four different surgical methods are in use: extrapleural pneumonectomy, pleurectomy/decortication, limited pleurectomy, and thoracoscopy with talc pleurodesis.
Extrapleural pneumonectomy is often used in the combination with radiotherapy. Radiotherapy is also used for palliation, especially in cases of pain. Sometimes the disease may regress, but significant improvement in survival has not been achieved.
Radiotherapy is usually given in combination with either surgery or chemotherapy, so the individual effects of the treatment modalities are difficult to document. Many different chemotherapeutic agents have been tested either as a single-agent treatment or in combination therapy.
In the best clinical series, objective responses are seen after single-agent therapy in about 20-30% of patients, but no significant effect on the overall survival. The best results in single-agent treatment have been achieved using anthracyclins, with doxorubicin giving up to a 40% response rate and high-dose cisplatin a response rate of up to 33%.
Rather promising results have been achieved also with carboplatin, epirubicin, ifosfamide, and mitomycin. High-dose methotrexate treatment resulted in a response rate of 37% in a study of 63 patients. Combinations of cisplatin, doxorubicin, or an alkylating agent like ifosfamide have been studied, usually, two or three drugs are combined.
No clear advantage over single-agent therapy has been observed. Combination therapy with cytokines, like interferon-á, has been disappointing despite the promising results in in vitro studies (Boutin et al., 1998). The resistance mechanisms of mesothelioma tumors have been studied only in a few publications and therefore remain largely unknown. Some of these studies will be discussed later.
Lung Cancer
Given the difficulties between the differential diagnosis of Malignant Pleural Mesothelioma and lung cancer, it has included experiments also on the biopsies and cell lines of lung cancer, mainly lung adenocarcinoma. The incidence of lung cancer is increasing due to the habit of tobacco smoking in the world. Over 3 million lung cancer deaths have been estimated worldwide in the year 2000.
In Finland 2 075 new lung cancer patients were diagnosed in 1994, after five years only 10% are still alive. Lung cancer is the second most common cancer among men in Finland.
The incidence among women is climbing and at present lung cancer is the second most common cause of cancer deaths among women. Tobacco is the most important etiological agent of all four subtypes of lung cancer responsible for approximately 90% of all cases.
Other known exogenous risk factors for lung cancer include asbestos, ionizing radiation, and other environmental carcinogens e.g. polycyclic aromatic hydrocarbons, nitrosamines, and aromatic amines.
The endogenous, host-related factors, include immunological factors and genetic predisposition mainly differences in carcinogen metabolism, DNA repair, and altered proto-oncogene and/or tumor suppressor gene expression.
Lung cancer is divided into two major classes mainly for treatment purposes: small cell lung cancer (SCLC) and non-small cell lung cancer (NSCLC). Virtually all cases arise from the epithelial tissue and are bronchogenic carcinoma subtypes. SCLC (30% of all lung cancers) proliferates fast, often sends metastases, and is primarily sensitive to anti-cancer drugs.
Therefore, the initial treatment is chemotherapy. However, resistance to treatment develops rapidly and many different resistance mechanisms have been speculated. P-glycoprotein cannot solely explain the clinical drug resistance and other possible drug resistance mechanisms include multidrug resistance proteins and decreased expression of topoisomerase II.
NSCLC comprises three histologically different carcinomas: adenocarcinoma (30-35%), squamous cell carcinoma (30-35%), and large cell anaplastic carcinoma (5%). The treatment of NSCLC is primarily surgery. Combination chemotherapies are widely used for the treatment of NSCLC since only 10-20% of the cases can be operated on.
In contrast to SCLC, NSCLC is primarily resistant to single chemotherapeutic agents. In adenocarcinoma, glutathione-related mechanisms have been suggested as potential resistance inducers along with other classical resistance mechanisms.
Reactive oxygen and nitrogen species
A free radical is defined as a chemical species that has a single unpaired electron in the outer orbital. In this state, the radical is extremely reactive and unstable. The most important radicals are the superoxide radical (O2-.), the hydroxyl radical (OH.), nitric oxide (NO.), and peroxynitrite (ONOO-). Reactive oxygen species (ROS) include free radicals and other oxygen-related reactive compounds, such as hydrogen peroxide (H2O2).
ROS are generated in normal aerobic metabolism in mitochondria, which are the main site of the production of radicals. In the cytosol and plasma membrane, ROS are formed by NADPH oxidase, cytochrome P450 oxidase, and xanthine oxidase. Transitional metals, such as iron and copper, are potential promoters of free radical damage, as they can convert superoxide, which in normal conditions is poorly reactive, into a rapidly reactive and highly toxic hydroxyl radical by Fenton chemistry.
In the Haber-Weiss reaction, hydroxyl radical is generated from O2 -. and H2O2. NO. has many useful physiological functions, but in excess amounts is a toxic-free radical as well. Many exogenous agents, such as hyperoxia, radiation, asbestos fibers, and ozone induce free radical formation in the cell.
Asbestos fibers cause oxidant production, directly and indirectly, one of the ways being catalysis by the ferrous iron, as asbestos fibers have high iron content. Inflammatory cells, such as neutrophils and alveolar macrophages, also produce large amounts of ROS when activated, especially when the phagocytosis is incomplete.
No production is also activated via the induction of inducible nitric oxide synthase by TNF and other cytokines released from the inflammatory cells. Reactive nitrogen species that are formed in reactions of NO. and oxygen/superoxide mediate the harmful effects of NO.
The pathological effects of ROS are wide-ranging; these toxic products can cause injury to practically to all cellular components. Lipid peroxidation of membranes, non-peroxidative mitochondrial damage, lesions in DNA, and cross-linking of proteins are the most relevant reactions of ROS leading to cell injury.
ROS are thought to be especially important in lung tissue that is exposed to much higher concentrations of oxygen than most other tissues but also to cigarette smoke and environmental pollutants. In addition to the toxic effects, ROS are important in non-toxic cellular reactions, including signal transduction
Antioxidants
To protect themselves from the harmful effects of oxidants, cells have several antioxidant enzymes and other antioxidant mechanisms. The latter include glutathione (GSH) and numerous GSHdependent enzymes, metal-binding proteins, and vitamins.
The three main types of antioxidant enzymes are the superoxide dismutases (SODs), catalase (CAT), and peroxidases, of which glutathione peroxidases (GPx) are thought to be the most important.
The SODs dis-mutate the superoxide radical into H2O2. GPx and CAT reduce H2O2 into water and oxygen. The glutathione redox cycle provides the cell with reduced glutathione (GSH) to act as a co-substrate for the peroxidases but to also participate in detoxification reactions and react nonenzymatically with OH and peroxynitrite.
Other enzymes involved in glutathione metabolism are glutathione reductase, glucose-6-phosphate dehydrogenase, glutathione S-transferases, and the enzymes participating in GSH-synthesis: -glutamylcysteine synthetase (GCS) and glutathione synthase (GS). Metal-binding proteins ferritin, ceruloplasmin, transferrin, haptoglobin, and albumin contribute to the antioxidant system by inactivating catalytic metals.
The most important antioxidant vitamins include -tocopherol, ascorbate, B-carotene, and flavonoids, but they will not be discussed in this review. Other enzymes with antioxidant capacity include cysteine-containing proteins such as the families of thioredoxin, glutaredoxin, and peroxiredoxin. These may play a role in the resistance of cells against oxidants but also against free radical generating drugs.
Superoxide Dismutases
Two main forms of SOD exist intracellularly: a copper-zinc-containing superoxide dismutase (CuZnSOD) and a manganese-containing superoxide dismutase (MnSOD). CuZnSOD is found in the cytoplasm and MnSOD in the mitochondria.
Extracellular SOD (EC-SOD) is in the extracellular matrix. MnSOD (also known as SOD2) is a homotetramer with a molecular weight of 88 000 and is in the mitochondrial matrix close to the electron transport chain, where ROS are produced in normal cellular metabolism.
The gene is in the long arm of chromosome 6 and is transcribed as two distinct mRNAs of 1 kb and 4 kb. MnSOD is synthesized in the cytoplasm as a precursor molecule containing a leader signal, which is removed during the transport of the molecule to the mitochondria.
Two polymorphic variants of MnSOD have been described, one leading to altered mitochondrial targeting of the enzyme and the other possibilities to changed MnSOD in vitro activity. The importance of MnSOD for normal physiology has been proven with knockout mice lacking the MnSOD gene, who died within 10-20 days of neurological manifestations and cardiotoxicity.
Heterozygous mice with half of the MnSOD activity have increased age-related mitochondrial oxidative damage. Approximately 15% of the total intracellular SOD activity is due to MnSOD. In eukaryotic cells, the MnSOD gene regulation is complex. The MnSOD promoter contains binding sites for several transcription factors such as AP1, AP2, SP1, and NF-B.
It has been hypothesized that the oxidative state of the cell is essential in regulating MnSOD expression. MnSOD is induced by the cytokine tumor necrosis factor (TN). TNF binds to its plasma membrane receptor, which initiates a series of events including intracellular ROS production, activation of NF-êB, and induction of the MnSOD gene. The TNF induction of MnSOD is blocked by the antioxidant N-acetyl cysteine (NAC).
Other factors that induce MnSOD are hyperoxia, irradiation, oxidized LDL, interleukin-1, interferon-, lipopolysaccharides, H2O2, and asbestos fibers. In some studies, the MnSOD gene induction is associated with resistance to hyperoxia, which would indicate that oxidant stress induces the enzyme to protect from subsequent oxidant injury. However, in contrast to many in vivo hyperoxia models, MnSOD is not directly upregulated by high oxygen tension in human bronchial epithelial cells in vitro.
In the human lungs, MnSOD is found in type II pneumocytes, bronchial epithelial cells, and alveolar macrophages. High levels of MnSOD are also found in the heart, brain, liver, and kidneys. In human malignancies, the role of MnSOD is controversial. In carcinogenesis, the antioxidant–oxidant imbalance is considered significant.
A polymorphism of the MnSOD gene resulting in an alteration in the transport of MnSOD into the mitochondria due to conformational change in the protein is a risk factor at least for the development of breast and lung cancers. Most studies have shown that MnSOD activity is low in cancer cells, and it has been proposed to be a cancer suppressor gene.
Transfection studies, in which only the MnSOD gene has been introduced, have shown a decreased level of malignancy and transformation of the malignant phenotype to the direction of a non-malignant one. However, the interpretation of this study is problematic as transfection creates imbalanced conditions in the cell.
On the other hand, at least gliomas, thyroid carcinomas, esophageal carcinomas, and colon carcinomas appear to contain high MnSOD levels when compared to the non-malignant tissues. In a study of five samples of lung tumors, the activity of total SOD was somewhat lower than in normal lung tissue. In Malignant Pleural Mesothelioma, MnSOD has not been previously studied before our group reported elevated activity of MnSOD in mesothelioma cell lines.
It has been reported that MnSOD is not inducible in cancer cells as it is in non-malignant cells (Wong & Goeddel, 1988) but also this issue is controversial. At least human lung adenocarcinoma cells show MnSOD induction by TNF. Human A549 lung cells also represent a malignant cell type but appear to show MnSOD induction.
CuZnSOD (SOD1) is a homodimer with a molecular weight of 32000 and is localized mainly in the cytosol, but it is also found in the nucleus and peroxisomes. The gene is in chromosome 21, the gene is transcribed as two mRNAs, 0.9 and 0.7 kb, respectively, the latter being the predominant form. In contrast to MnSOD, CuZnSOD-deficient animals and cells are viable, but they are sensitive to oxygen toxicity. Mutation of this gene is associated with familial amyotrophic lateral sclerosis.
The regulation of CuZnSOD also differs from MnSOD, e.g. its level is constitutive in several animal studies and human lungs, and neither is it induced by hyperoxia, TNF, or interleukin-6. In a healthy human lung, CuZnSOD is found in the bronchial epithelium.
High levels are also found in the liver, erythrocytes, brain, and neurons. In a recent study, the CuZnSOD gene was found to be upregulated in a mesothelioma cell line compared to a non-malignant mesothelial cell line when assessed in a microarray containing over 6900 genes.
Otherwise, its expression and role in human tumors remain unclear. EC-SOD is a copper and zinc-containing homotetrameric glycoprotein. It is in the extracellular matrix in all human tissues and its gene is in chromosome 4. EC-SOD is induced by cytokines like TNF, direct oxidant stress does not affect ECSOD as it does MnSOD.
EC-SOD is concentrated in pulmonary vessels and airways and found in systemic arteries. Of the pulmonary cell types, it is found in bronchial epithelium, alveolar macrophages, and endothelial cells. Its role and regulation in cancer are unknown.
Glutathione
Glutathione is the predominant intracellular low molecular weight thiol in all mammalian cells. It is usually present in the mill molar range; the intracellular level is approximately 1-8 mm and the extracellular level is typically 5-50 M. About 99% of the intracellular glutathione is in the reduced form
Approximately 85% of the intracellular glutathione is in the cytosol, about 15% in the mitochondria, and a small percentage in the endoplasmic reticulum. The mitochondrial GSH pool is maintained by the activity of a mitochondrial transporter that translocates cytosolic GSH into mitochondria.
GSH is a central protective antioxidant against free radicals and other oxidants, but it has also an essential role in detoxification reactions. Other cellular events where glutathione is considered valuable are modulation of redox-regulated signal transduction, regulation of cell proliferation, remodeling of extracellular matrix, apoptosis, mitochondrial respiration, and a reservoir of cysteine.
Numerous studies show that resistant human cancer cell lines contain high glutathione levels in vitro and that oxidant-induced toxicity can be enhanced by buthionine sulfoximine (BSO) which causes glutathione depletion by inhibiting its synthesis. The role of glutathione in oxidant and drug resistance has not been previously investigated in Malignant Pleural Mesothelioma
Enzymes in the glutathione redox cycle: Glutathione peroxidase (GPx) and glutathione reductase (GR)
GPx is one of the major enzyme families in removing hydrogen peroxide generated by, e.g., superoxide dismutases. It catalyzes the reaction where GSH is oxidized into GSSG and H2O2 converted into water and oxygen. Four distinct selenoproteins are included in the family of glutathione peroxidases, the classical form being the cytosolic GPx, which is also found in the mitochondria and extracellular matrix.
The other three are the gastrointestinal form of GPx, a non-selenium-dependent GPx, and phospholipid hydroperoxide GPx. The cytosolic GPx, a tetrameric selenoprotein, has a molecular weight of 85 000. The gene is on chromosome 3. Recently a polymorphism was found that is associated with lung cancer.
In normal physiological conditions with low or moderate production of H2O2, GPx has been considered a more important scavenger than catalase, because its Michaelis-Menten constant (Km value) for H2O2 is lower than that of catalase. Selenium is needed in the synthesis of GPx and at least the extracellular GPx is induced by hyperoxia and oxidants.
GPx is ubiquitously expressed in erythrocytes, kidneys, and the liver. The expression of GPx in malignant tumors is somewhat variable. GPx activity has been suggested to be elevated in adenocarcinoma of the lung. Whereas it was decreased in other lung cancer subtype biopsies when assessed by immunohistochemistry.
Elevated GPx activity has been linked with chemoresistance of anticancer drugs, such as adriamycin, which kills cells by releasing free radicals. Glutathione reductase (GR) converts GSSG back to GSH at the expense of NADPH forming a redox cycle. Two isoenzymes of GR, one cytosolic and one mitochondrial, are encoded by a single gene located in chromosome 8.
It has been postulated that the glutathione conjugates formed in xenobiotic detoxification can inhibit GR thereby accumulating GSSG and altering the redox capacity of the cell. The expression of GR in human lungs and tumors is unclear.
Enzymes in glutathione biosynthesis
-glutamylcysteine synthetase (GCS) is the rate-limiting enzyme in GSH biosynthesis. The synthesis requires another ATP-dependent enzyme, glutathione synthase, and the amino acids glutamic acid, cysteine, and glycine. In general, the activity of GCS defines the rate of glutathione synthesis and GCS is feedback-inhibited by the product, GSH.
Cysteine is the rate-limiting substrate. Levels of GSH and cysteine are the two factors that regulate the synthesis of glutathione under physiological conditions. The importance of glutathione synthesis was proven in a recent study which showed that homozygous knockout mouse lacking the GCS heavy subunit gene dies before birth.
GCS is a cytosolic heterodimer consisting of a heavy subunit (GCSh, MW~ 73 000) and a light subunit GCSl, MW ~30 000. GCSh gene is in chromosome 6 (6p12) and GCSl gene in chromosome 1 (1p21) and two mRNA transcripts are consistently seen for both subunits. GCSh is the catalytically active subunit; it also binds the feedback inhibitor GSH.
It has been suggested that GCSh alone comprises about half of the enzyme activity when compared with the holoenzyme. Some studies, however, have concluded that it has no catalytic activity without the light subunit. GCSl serves an important regulatory role and reduces the inhibitory effect of GSH.
It has been suggested that during GSH depletion, in oxidizing conditions, the enzyme undergoes conformational changes between subunits that allow an increase in enzyme activity. In normal physiological conditions when abundant amounts of GSH are present, both subunits are needed for the enzyme activity. GCS is induced by several agents, including oxidants e.g. H2O2 and menadione, cytokines e.g. TNF, heavy metals e.g. cadmium and iron, and some chemotherapeutic agents e.g. cisplatin.
At the transcriptional level, GCS subunits are regulated by several regulatory signals, including ARE, TRE, AP1, and NF-B. GCS activity is also regulated at the post-transcriptional and translational level, and phosphorylation/dephosphorylation may control its activity. Possible inhibitors include glucocorticoids, insulin, prostaglandin E, and TGF-.
Exposure to sublethal doses of oxidants may initiate an adaptive antioxidant response, where the intracellular GSH is first depleted leading to oxidant stress and consequent GCS upregulation. The role of -glutamyl transpeptidase in regulating GCS activity indirectly by cleaving extracellular GSH has also been suggested. The expression of GCS mRNA varies between different tissues.
In healthy human lungs, GCS mRNA has been detected from bronchial epithelial cells. There are no previous studies on the expression or distribution of GCS in malignant tumors. It has been suggested that chromosome 1 (loss of 1p21-22) is often deleted in Malignant Pleural Mesothelioma.
This would predispose an individual to the development of the tumor. Elevated levels of GCS have been detected in many drug-resistant malignant cell lines. Chemoresistance may be associated with the accumulation of GSH, which functions as an antioxidant but is also used in detoxification reactions.
Glutathione has also been shown to inhibit apoptosis by changing the redox state of the cell. Apoptosis resistance, in turn, has been considered important in the drug resistance of malignant cells. Glutathione synthase (GS) is a cytosolic homodimer that catalyzes the reaction of L- -glutamyl-L-cysteine and glycine that forms GSH.
GS is composed of two apparently identical subunits (each MV~52 000) and the gene is in chromosome 20. Two forms of glutathione synthetase deficiency have been described. One form is mild, causing hemolytic anemia, but the other more severe form causes 5-oxo-prolinuria with secondary neurological involvement. The regulation of GS is poorly known.
In glutathione biosynthesis, the availability of cysteine is crucial. Cysteine is transported into the cell by a sodium-dependent A system and cystine, an oxidized form of cysteine, by an inducible transporter Xc-. Cystine is then reduced to cysteine that can be used in GSH biosynthesis. The transport of cystine is induced by oxidants, such as hyperoxia and H2O2, contributing to increased GSH levels during oxidative stress.
There are no studies on the expression of GS or cysteine transporters in malignant tumors. glutamyl transpeptidase (GT) acts as a salvage enzyme in GSH synthesis. The molecular weight is 50 kD for the heavy and 25 kD for the light subunit (Arai et al., 1995). The gene is on chromosome 22. GT is located on the plasma membrane, where it cleaves the -glutamyl bond in extracellular -glutamyl cysteinyl-glycine.
The amino acids are returned to the cell and reused for GSH synthesis. GT is induced by menadione and t-butyl hydroquinone, suggesting its role in protecting cells during oxidative stress. In addition to other luminal surfaces of the body, lung epithelium contains high levels of this enzyme.
There is one study showing that mesothelioma biopsies are negative for this enzyme when assessed by immunohistochemistry. In the same study, strong immunoreactivity is detected in renal cell carcinoma, adenocarcinoma of the prostate, and papillary carcinoma of the thyroid.
Glutathione S-transferases (GSTs)
GSTs are a superfamily of detoxifying enzymes that have broad substrate specificities. Five families of cytosolic GSTs have been identified in humans, of which four have been thoroughly characterized: Alpha, Mu, Pi, and Theta. The genes for GST-class are all located in chromosome 1, whereas GST-the gene is in chromosome 11. A polymorphism of GSTM1 (-class) resulting in dysfunction of the enzyme has proven to be a risk factor for malignant diseases, including mesothelioma.
The GSTs conjugate GSH with compounds containing an electrophilic center and thereby provide critical protection against xenobiotics and products of oxidative stress. Since the GSH-conjugate is transported out of the cell, intracellular GSH is consumed irreversibly in the conjugation and thus maintenance of intracellular GSH levels is essential for the optimal function of GSTs.
Many GST enzymes possess GPx activity as well. Many of the substrates of GSTs also induce the expression of the GST genes, suggesting an adaptive response to chemical stress. Carcinogens and alkylating agents may induce GST-.
The GST-ð family is the predominant GST in human solid tumors and has even been used as a marker in the lung, colon, bladder, and other human cancers (Zhang et al., 1998). GST activity is often associated with anticancer drug resistance, as the drugs are converted to a less toxic form by conjugation. Based on one study 77% of mesothelioma cell lines expressed GST in immunohistochemistry.
Catalase
Catalase (CAT) is a tetrameric hemoprotein that catalyzes the reaction of decomposition of H2O2 into water and oxygen. It has a molecular weight of 240 000. It is mainly localized in the peroxisomes (Davies et al., 1979) but is also found in the cytoplasm and mitochondria in minor amounts. The gene is localized in chromosome 11. Patients suffering from acatalasemia have a mutation of the CAT gene but are clinically healthy.
Catalase has a higher Km than GPx, which suggests a major role for CAT at higher levels of H2O2 but a minor role at physiological levels of H2O2. Catalase is not abundantly present in the mitochondria, where the physiological oxidative stress is at its highest. It has been shown to be induced by high oxygen tension in alveolar epithelial cells.
In other studies, however, no induction could be detected in lung epithelial cells after oxidant or cytokine exposures. There are no systematic studies on catalase in malignant tumors. Some studies have suggested variable catalase expression in lung, breast, and colon cancers. One recent study showed that catalase is highly expressed in Malignant Pleural Mesothelioma. No major role has been suggested to catalase in drug resistance.
Other proteins with antioxidant capacity
Glutaredoxin and peroxiredoxins are cysteine-containing H2O2-scavenging proteins, that have been recently described, but no investigations of these proteins have been conducted in human lung tumors. Thioredoxin is composed of two closely related cysteine-containing proteins, thioredoxin (TRX) and thioredoxin reductase (TRXR).
This group of proteins enhances cell proliferation and increases resistance to apoptosis in several in vitro and in vivo experimental models. There are two recent studies showing overexpression of TRX and TRXR in lung tumors and mesothelioma (Kahlos et al., 2001a; Soini et al., 2001a). However, the expression of these proteins did not correlate with survival in either tumor. Heme oxygenase (heat shock protein 32) has also been shown to have antioxidative properties.
-
Read More – Mesothelioma Symptoms, Diagnosis, and Treatment / How to Take Good Sleep /
-
Affiliate Products: